Personalised medicine and Genomics are groundbreaking advances in healthcare that effort to personalised medical treatment constructed on specific genetic profiles. This chapter explores into the fundamental principles, technological advancement, applied uses, benefits, complications, and diagnoses of genomics and tailored medicine.
Fundamental concepts
1. Genomics:
iIt s the scientific discipline that investigates the entirety of an organism’s DNA, known as its genome. This research field encompasses examining the genome’s structure, function, evolution, and mapping. Genomic analysis involves studying all genes and their connections to understand their impact on health and disease.
2. medicine, commonly called precision medicine:
It entails customising medical therapy based on the unique characteristics of all patients. This method considers genetic, environmental, and behavioural aspects to create therapies that are more efficient and focused.
3. Technological progress
1. Next-generation sequencing (NGS) refers to advanced technologies that enable fast and thorough sequencing of complete genomes or particular sections of the genome. Genome sequencing has been significantly transformed by this advancement, leading to increased speed, reduced cost, and improved accessibility in genetic research and diagnostics.
Illumina’s Next-Generation Sequencing (NGS) technologies are extensively utilised for whole-genome sequencing, facilitating meticulous examination of genetic variants and mutations.
2. CRISPR-Cas9 is a gene-editing tool.
Clustered regularly interspaced palindromic repeats (CRISPR)/Cas9 is an innovative technique for editing genomes that enables accurate alterations to DNA. It possesses the capacity to rectify genetic mutations and address genetic illnesses at their origin, It makes it possible to correct errors in the genome and turn on or off genes in cells and organisms
CRISPR Therapeutics is now engaged in the development of treatments using CRISPR technology specifically designed for illnesses such as sickle cell disease and beta-thalassemia.
3. Bioinformatics is the application of computing technologies to analyse and interpret biological data. Managing and analysing the large quantities of data produced by genetic investigations is crucial.
The Human Genome Project extensively utilised bioinformatics to accurately map and comprehend the human genome.
Software programs or computer applications.
1. Medical intervention for the treatment of cancer:
By doing genomic profiling of tumours, it is possible to identify precise mutations that are responsible for driving the growth of cancer. This knowledge allows for the creation of medicines that specifically target these mutations. This method enhances the effectiveness of treatment and minimises the occurrence of adverse effects.
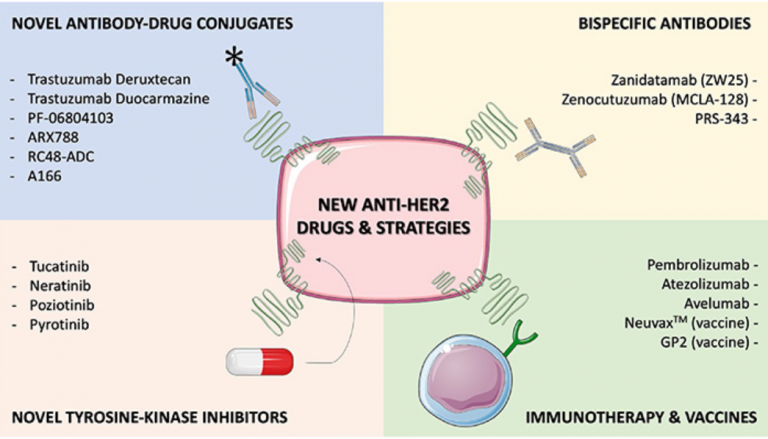
2. An instance of personalised medicine that has achieved success is the utilisation of Human epidermal growth factor receptor 2, HER2-targeted treatments such as trastuzumab (Herceptin) in cases of HER2-positive breast cancer.
Pharmacogenomics is the field of study that investigates the influence of genes on an individual’s reaction to medications. It aids in the selection of appropriate drugs and doses for individual patients, reducing negative side effects and maximising therapeutic advantages.
The US Food & Drugs Administration (FDA) advises doing genetic testing before administering the anticoagulant warfarin to ascertain the most suitable dosage and minimise the likelihood of bleeding problems.
3. Rare genetic disorders can be diagnosed using whole-exome sequencing and whole-genome sequencing, which can pinpoint the specific genetic abnormalities responsible for the condition. This allows for earlier and more precise diagnosis.
Example: Diagnosing cystic fibrosis by detecting mutations in the CFTR gene.
Prenatal and newborn screening involves the use of genomic testing to detect genetic abnormalities in fetuses and infants. This enables timely intervention and treatment of hereditary disorders.
4. Non-invasive prenatal testing (NIPT) is a screening method used to detect chromosomal abnormalities, such as Down syndrome.
Benefits
1. Enhanced Treatment Results:
Personalized medicine enhances the probability of effective treatment by tailoring medicines to an individual’s genetic profile, hence minimising the need for tests and mistakes in medication selection.
2. Decreased Adverse Reactions:
Through comprehension of genetic characteristics, healthcare personnel could refrain from giving medications that potentially induce significant side reactions in specific patients.
3. Healthcare Prevention:
Genomic details could be exploited to identify patients with a heightened susceptibility to specific illnesses, allowing for preventive interventions and modifications to their lifestyle to avert the start of these maladies.
4. Optimal Resource Utilization:
Targeted therapy can achieve greater cost-efficiency over time by minimising the necessity for expensive and repetitive treatments.
Challenges
1. Ethical and privacy concerns: It is crucial to prioritise informed permission, privacy of information, and safeguarding from discrimination based on genetics.
2. Data interpretation: Treatment and diagnosis decisions can be challenged by variants of uncertain significance (VUS).
3. Cost and Accessibility: Although there has been a decline in the cost of genome sequencing, it still retains prohibitively exorbitant for a significant number of patients. Achieving fair and equitable accessibility to genetic medicine is a substantial obstacle.
4. Incorporating genetic information into routine clinical procedures:
It necessitates educating medical professionals and establishing uniform processes.
Future Directions
1. Developments in Genome Editing: Ongoing progress in genome-editing technologies such as CRISPR will broaden their therapeutic uses, potentially leading to the eradication of genetic disorders.
2. The expansion of personalised medicine is expected to occur as genomic databases continue to expand and our knowledge of hereditary impacts on health advances. This will lead to the integration of personalised medicine into mainstream healthcare practices.
Artificial Intelligence (AI) and Machine Learning (ML) will have a pivotal role in examining intricate genomic data, detecting patterns, and forecasting the likelihood of diseases and the effectiveness of treatments.
4. Global genetic Initiatives: International partnerships, such as the Global Alliance for Genomics and Health (GA4GH), will improve data exchange and facilitate research, speeding up scientific breakthroughs and the adoption of genetic healthcare on a global scale3.
Scaling healthcare globally, particularly at a “Scale 3,” denotes moderate yet substantial global initiatives or programs that address health concerns. This could entail the following:
Targeted Interventions, Capacity Building, Technology Deployment, Health Education and Prevention, Partnerships and Funding, Data and Monitoring, Policy and Advocacy, and Strengthening Local Health Governance
“Scale 3” implies a concentration on substantial, focused health interventions that, despite their limited global reach, have a significant regional or multi-country impact. These efforts are crucial for addressing specific health challenges strategically and effectively.
Conclusion
Genomics and personalised medicine are leading the way in a medical revolution, providing the potential for customised medicines that are both more efficient and have reduced negative effects. Notwithstanding the difficulties, the continuous progress in technology and research is creating a path towards a future where health is genuinely tailored to individual needs. To fully unlock the potential of genomes and personalised medicine, it is crucial to overcome ethical, operational, and educational obstacles. Doing so will result in substantial enhancements in medical treatment and results.
